
Rux dose for 65 yo, symptomatic high-risk MF, platelet count 35K/µL? Platelet count 70K/µL?
Rux dose for 65 yo, symptomatic high-risk MF, platelet count 35K/µL? Platelet count 70K/µL?
A 65-year-old patient with high-risk myelofibrosis, splenomegaly, normal renal function and disease-related symptomatology is being considered to receive ruxolitinib for the first time. What dose would you initiate in each of the following scenarios (or would you not use it)?
| Platelet count | Hgb | WBC |
Usual Tx (+/- corticosteroids) for pts w/ asymptomatic MF but w/ anemia?
Usual Tx (+/- corticosteroids) for pts w/ asymptomatic MF but w/ anemia?
What treatment would you usually recommend for patients whose MF is asymptomatic but who have anemia?
Initial Tx for 65 yo, int-2, sympt MF, baseline anemia? High-risk MF, anemia develops on Rux: Adjust dose?
Initial Tx for 65 yo, int-2, sympt MF, baseline anemia? High-risk MF, anemia develops on Rux: Adjust dose?
Which treatment would you most likely initiate for a 65-year-old patient with intermediate-2 myelofibrosis, splenomegaly and significant disease-related symptomatology who has already received EPO and danazol:
| Platelet count | Hgb | WBC |
| 220,000/µL |
Additional Commentary
Additional Commentary:
What is the role of iron chelation for patients with MF who have frequent transfusion requirements?
Additional Commentary
Additional Commentary:
How common is the occurrence of hydroxyurea-related leg ulcers?
Additional Commentary
Additional Commentary:
Is hydroxyurea considered leukemogenic?
Additional Commentary
Additional Commentary:
Is there cross-resistance between ruxolitinib and other JAK2 inhibitors?
Additional Commentary
Additional Faculty Comments:
GICU113
OVERVIEW OF ACTIVITY
Consensus or Controversy, Issue 2: Clinical Investigators Provide Their Perspectives on Controversial Issues in the Management of Myelofibrosis
COCMF13/2
TARGET AUDIENCE
This activity is intended for medical oncologists, hematologist-oncologists, hematology-oncology fellows, oncology nurses and other practitioners involved in the management of myelofibrosis.
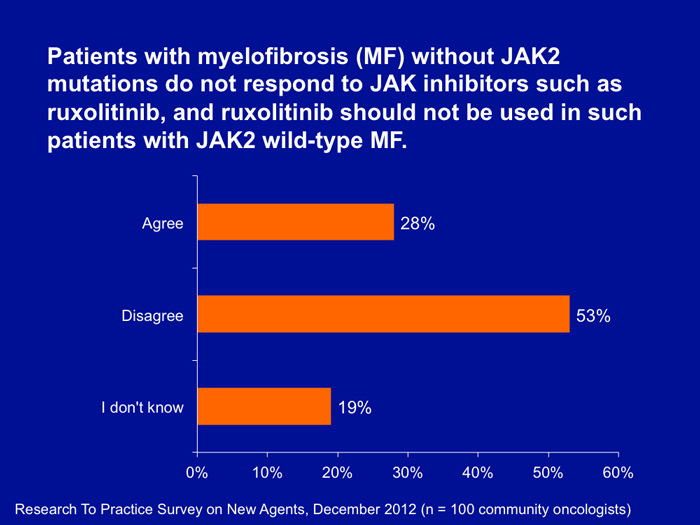
Patterns of Care Data Regarding Ruxolitinib Use in Patients without JAK2 Mutations
Patterns of Care Data Regarding Ruxolitinib Use in Patients without JAK2 Mutations
Additional Commentary
Allotransplant in patients with MF?
In what situations, if any, do you recommend allotransplant to patients with MF?
Additional Commentary
Splenectomy in patients with MF?
Presently, how often do you recommend splenectomy to patients with MF?
Additional Commentary
Other diseases most commonly confused with MF?
Based on your clinical experience, which of the following disease states is most often confused with a diagnosis of myelofibrosis (MF)?