Email from the Editor
Click here to go directly to the web- and video-based education resources related to this week’s topic
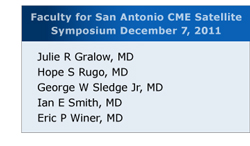 In 2 weeks, on Wednesday night, December 7 in San Antonio we will host another adventure in CME with a satellite symposium featuring discussion of actual current cases of patients with breast cancer. Maybe it’s because my body seems to be falling apart from what appears to be the early stages of old age or perhaps it’s related to the fact that every time we ask oncologists to present tough clinical situations they immediately bring up patients older than age 90, but my favorite case to be presented in San Antonio is an 88-year-old otherwise spry and healthy woman with metastatic triple-negative breast cancer. In describing this individual and her situation, the patient’s oncologist, Dr Alejandra Perez of Hollywood, Florida, seemed almost apologetic when she revealed that this woman of clearly advanced age had received 5 lines of chemotherapy. Interestingly, however, each time the patient tolerated treatment well, and Dr Perez was eager to learn how the faculty might have approached this provocative situation.
In 2 weeks, on Wednesday night, December 7 in San Antonio we will host another adventure in CME with a satellite symposium featuring discussion of actual current cases of patients with breast cancer. Maybe it’s because my body seems to be falling apart from what appears to be the early stages of old age or perhaps it’s related to the fact that every time we ask oncologists to present tough clinical situations they immediately bring up patients older than age 90, but my favorite case to be presented in San Antonio is an 88-year-old otherwise spry and healthy woman with metastatic triple-negative breast cancer. In describing this individual and her situation, the patient’s oncologist, Dr Alejandra Perez of Hollywood, Florida, seemed almost apologetic when she revealed that this woman of clearly advanced age had received 5 lines of chemotherapy. Interestingly, however, each time the patient tolerated treatment well, and Dr Perez was eager to learn how the faculty might have approached this provocative situation.
Perhaps not surprisingly, during our last breast cancer symposium held in Chicago during ASCO we discussed a number of issues relevant to this clinical scenario. Below we present the perspectives (text-based and video) of our 8 faculty members, but it will be interesting to see if any of this changes a couple weeks from now in the city by the river.
1. Systemic treatment in patients with metastatic triple-negative disease (and patients with ER-positive, HER2-negative tumors who no longer respond to hormones)
The debate continues about bevacizumab, and at our event Dr Bob Carlson (click here for an 89-sec video) reviewed the discussions he has been a part of as chair of the NCCN breast cancer guidelines committee and reiterated their stance that bev plus chemo remains an acceptable evidence-based option despite regulatory controversy about this. Importantly, as we were authoring this commentary, the FDA formally removed approval of this agent in breast cancer, thus adding another wrinkle to the debate and further calling into question who is in the best position to decide how patients should be treated. On a related note, Dr Joyce O’Shaughnessy (38 sec) commented on the recent positive clinical data with bev in triple-negative disease and speculated that this may correlate with the elevated serum VEGF-A levels seen in these patients. In terms of choice of first-line therapy in everyday clinical practice, most of our faculty start with a taxane and in patients with BRCA mutations a platinum agent is also often employed.
2. Integration of new agents into the treatment algorithm
During this discussion, Dr O’Shaughnessy (114 sec) also focused on one of the newest additions to the systemic treatment algorithm, the sea sponge derivative/microtubule inhibitor eribulin and the key clinical data demonstrating a rare survival advantage in a trial for metastatic disease. This topic spurred a provocative faculty interchange (70 sec) about clinical trial design that culminated with Dr Martine Piccart-Gebhart (133 sec) voicing her deep concern that the survival bar seemingly set by regulatory agencies will discourage industry from developing new agents in breast cancer, in which the downstream effects of treatment often make survival benefits very challenging to achieve. Dr Eric Winer believes that eribulin may be the last chemotherapy drug approved for metastatic breast cancer, and all of our faculty members recognize its potential benefit and currently use the agent in their practices.
3. Endocrine treatment in patients with disease recurrence while receiving adjuvant hormones
For the first time in years I am pumped up about an endocrine presentation — specifically the first plenary of SABCS — during which the results of the Phase III SWOG-S0226 trial comparing an AI to an AI with fulvestrant in metastatic disease will be unveiled. Endocrine maven Professor John Robertson has for years been talking on our audio programs about this “total estrogen blockade” strategy, and having not been able to bribe or sweet-talk any of the SWOG investigators into giving us a preview of what will be presented, we will all just have to wait. I wouldn’t be surprised if the study is flat-out negative or demonstrates a big bump in maybe progression-free survival, and if that is the case perhaps practice will change and new adjuvant trials will be launched evaluating this concept. But before we get ahead of ourselves, in terms of current management, when confronted with a premenopausal patient with disease progression on adjuvant tamoxifen, the faculty commonly use ovarian suppression and an AI. For postmenopausal patients experiencing relapse on a nonsteroidal AI it’s either fulvestrant or exemestane.
Next up, in the last of our breast cancer miniseries: HER2 not included, part 2 — adjuvant treatment, genomic biomarkers, bone-targeted agents and more.
On a closing note, almost everyone is aware of the 2 major conferences coming up (ASH and SABCS), but another cool event is taking place December 1-3 in D.C. that our colleague and super good guy Dr John Marshall from the Lombardi Cancer Center is hosting. Titled Fighting a Smarter War Against Cancer, this unique symposium (for those of you not trudging out west for the ASH/San Antonio craziness) will feature major stakeholders delving into the provocative concept of value in cancer care.
Neil Love, MD
Research To Practice
Miami, Florida