
Email from the Editor
Click here to go directly to the web- and video-based education resources related to this week’s topic
Recently, my favorite Michigan Wolverine Dr Dan Hayes sent me an email query as to whether we had any Patterns of Care data he might use in an editorial he was writing for Nature Reviews. Dr Hayes had been asked to comment on a recent JCO paper discussing the estimated 9% of Phase III trials presented at ASCO but never published in peer-reviewed publications. What Dan wanted to know was if we had any specific examples of how presented but unpublished data sets change clinical practice.
In analyzing our prior survey results we came across a number of instances in which this was precisely the case. Perhaps the most striking example related to the use of adjuvant trastuzumab (T) for the treatment of HER2-positive breast cancer. In February 2005 we asked 200 community oncologists a variety of questions, including how they would care for a patient with a HER2-positive tumor and positive nodes. At that time only 4% would have used T. In August, when we presented the same question to a separate cohort of oncologists, 96% stated they would use T.
As we all know, what precipitated this dramatic shift was the historic ASCO “education session” on May 16, during which 3 major adjuvant T trials were presented. As these studies were not formally published until October, it becomes apparent that medical oncologists will act quickly when important research data are presented. In his editorial, Dan argues passionately that despite this “rapid response system,” patients who participate in large Phase III trials deserve to see their experiences registered using the best method we now have to put new data into perspective: The peer review system. Amen.
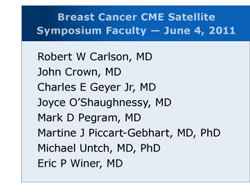 In this, the first of 3 issues of our peripatetic Consensus or Controversy series focused on breast cancer, we check in with 8 prominent investigators about their current HER2 management practices 6 years after the aforementioned 2005 data explosion. These and many other related issues were explored as part of a live CME symposium we hosted in Chicago during the most recent ASCO (click for the video proceedings), and below we present the bottom line on the investigators’ perspectives along with a few highlight video clips from the meeting to spice up your read:
In this, the first of 3 issues of our peripatetic Consensus or Controversy series focused on breast cancer, we check in with 8 prominent investigators about their current HER2 management practices 6 years after the aforementioned 2005 data explosion. These and many other related issues were explored as part of a live CME symposium we hosted in Chicago during the most recent ASCO (click for the video proceedings), and below we present the bottom line on the investigators’ perspectives along with a few highlight video clips from the meeting to spice up your read:
1. Adjuvant treatment today (click here for investigator preferences)
As eloquently recounted during the symposium by BCIRG participants Drs Mark Pegram and John Crown (click here for a 40-second video clip), whether or not to use an anthracycline with T remains controversial. However, in the just-published (finally) BCIRG 006 trial, a trend for slightly fewer recurrences was seen in the AC ![]() docetaxel/T arm. Perhaps as a result, 7 of 8 faculty members include an anthracycline for younger patients with node-positive tumors. On the other hand, Dr Chuck Geyer (44 sec) cautions us that older patients, particularly those with borderline ejection fractions and cardiovascular risk factors, have a substantially higher risk of a cardiac event and in those cases he chooses TCH.
docetaxel/T arm. Perhaps as a result, 7 of 8 faculty members include an anthracycline for younger patients with node-positive tumors. On the other hand, Dr Chuck Geyer (44 sec) cautions us that older patients, particularly those with borderline ejection fractions and cardiovascular risk factors, have a substantially higher risk of a cardiac event and in those cases he chooses TCH.
Another major continuing debate relates to the management of smaller node-negative tumors. Many investigators continue to rely on the 5-mm bar as the cutoff for the use of chemo/T, yet Dr Joyce O'Shaughnessy (29 sec) often considers ER status when making these decisions and is more likely to use chemo/T in patients with ER-negative tumors.
2. Adjuvant treatment soon?
Six years later, at least 2 major next-generation randomized HER2 studies have accrued and hopefully will report in the not-so-distant future. The NSABP BETH trial added bevacizumab to TCH, and the international ALTTO trial evaluated chemo with T or lapatinib (L) alone, in sequence or the combination. During our symposium Dr Michael Untch (73 sec) commented that in his German GEPARQUINTO neoadjuvant trial, L was inferior to T in terms of path CR rate (and tolerability). Perhaps this syncs up with the recent news that ALTTO closed the L alone arm due to futility. It is interesting to note that all of the faculty members are currently using the T/L combination in metastatic disease, and we shall soon see if this approach is beneficial in the adjuvant setting.
3. Octogenarians and beyond
The problem here, of course, is the use of chemotherapy. However, most of the investigators we asked generally do not consider T alone. Thus, if treatment is administered the faculty often turns to paclitaxel/T, a regimen currently being studied at Dana-Farber as described by Dr Eric Winer (51 sec).
4. Metastatic disease (click here for investigator preferences)
The faculty embraces the concept of indefinite anti-HER2 blockade in these patients, and there are a host of new agents with known activity providing even more hope for the future. In San Antonio next month we will get our first look at the results from the Phase III CLEOPATRA trial evaluating the combination of T and pertuzumab, a monoclonal antibody that inhibits dimerization of HER2, and at our satellite Dr Winer (67 sec) discussed another exciting candidate, the antibody-drug conjugate T-DM1, which seems most noteworthy for its lack of chemotherapy-like side effects despite clear-cut efficacy. All of our faculty and for that matter every breast cancer investigator is ready now to use this agent in metastatic disease. Unfortunately, it seems like that will not be possible for quite some time.
Next up on this breast cancer miniseries: The other 80% of breast cancer, the HER2-negative subset, as we discuss the management of metastatic disease, including the sequencing of endocrine agents and cytotoxics.
Neil Love, MD
Research To Practice
Miami, Florida